Measles Outbreaks and the Policy Choices Behind Them
Measles, once eliminated in the U.S., is resurging due to declining vaccination rates, misinformation, and gaps in public health policy, putting communities at risk of preventable outbreaks.
THE DILEMMA
Should states eliminate non-medical vaccine exemptions to prevent measles outbreaks?
Measles is spreading due to low vaccination and policy gaps.
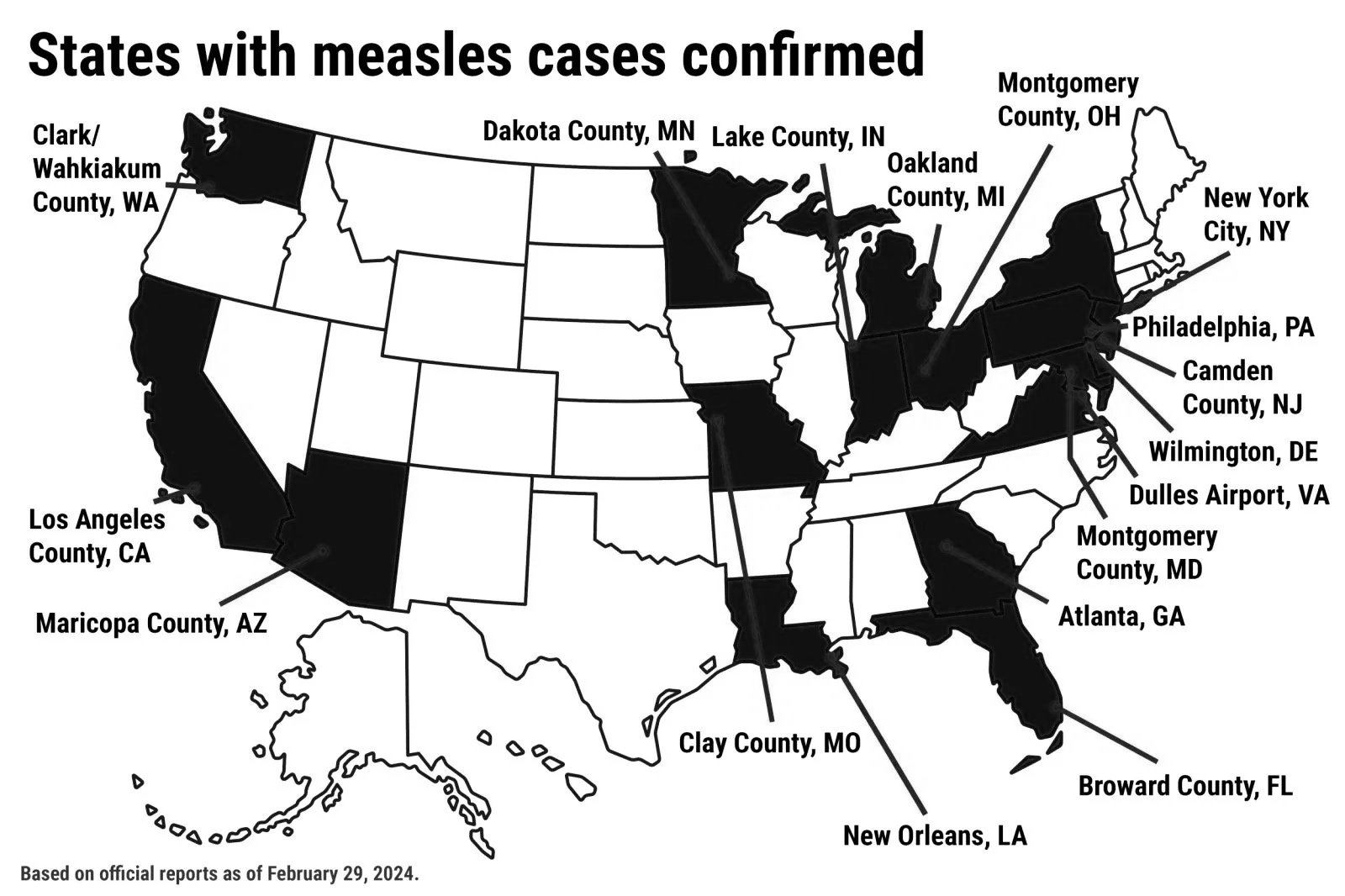
Measles, a disease once eliminated from the United States, is making a troubling comeback. In 2026, dozens of states have reported outbreaks, raising alarms among public health officials and communities. The resurgence is largely driven by declining vaccination rates in certain areas, fueled by misinformation about vaccine safety and lenient state exemption laws. Measles is highly contagious and can lead to serious complications such as pneumonia, encephalitis, and even death, making these outbreaks especially concerning. Policy decisions play a critical role in determining how widespread and severe these outbreaks become. States that allow non-medical exemptions for vaccines often see lower immunization coverage, creating pockets where measles can easily spread. Federal and state funding for public health programs has also been inconsistent, limiting efforts to educate communities about the importance of vaccination and to provide access to vaccines in underserved areas. International travel further complicates the issue, as measles can be imported from countries where the virus remains common. Addressing the resurgence requires coordinated policy action. Strengthening school vaccination requirements, increasing funding for immunization campaigns, and implementing strategies to combat misinformation are all essential steps. Healthcare providers also play a key role by encouraging vaccination and educating patients about the risks of preventable diseases. The return of measles demonstrates that public health successes can be fragile when policy, education, and access do not align. Protecting communities from preventable diseases requires constant attention to both policy and public engagement.
Works Cited
Government & Official Data
Centers for Disease Control and Prevention (CDC). Measles Cases and Outbreaks in the United States, updated 2026. Data show confirmed measles cases in multiple states and reduced vaccination coverage below herd immunity thresholds.
2. News & Reports on Measles Trends
U.S. measles cases in 2025 reached the highest level in decades, with over 2,000 confirmed infections and hospitalizations, largely among the unvaccinated.
The United States is at risk of losing its measles elimination status due to sustained outbreaks and declining vaccine uptake.
3. Scientific & Research Findings on Policy Impacts
Stanford Medicine research indicates falling childhood vaccination rates increase the risk of measles becoming endemic in the U.S. without policy intervention.
Johns Hopkins study finds that state policies allowing non-medical vaccine exemptions are linked to lower MMR vaccination coverage.
4. Expert & Global Context
The Global Virus Network warns of measles resurgence in the U.S. and worldwide, emphasizing the importance of vaccination to prevent disease spread.